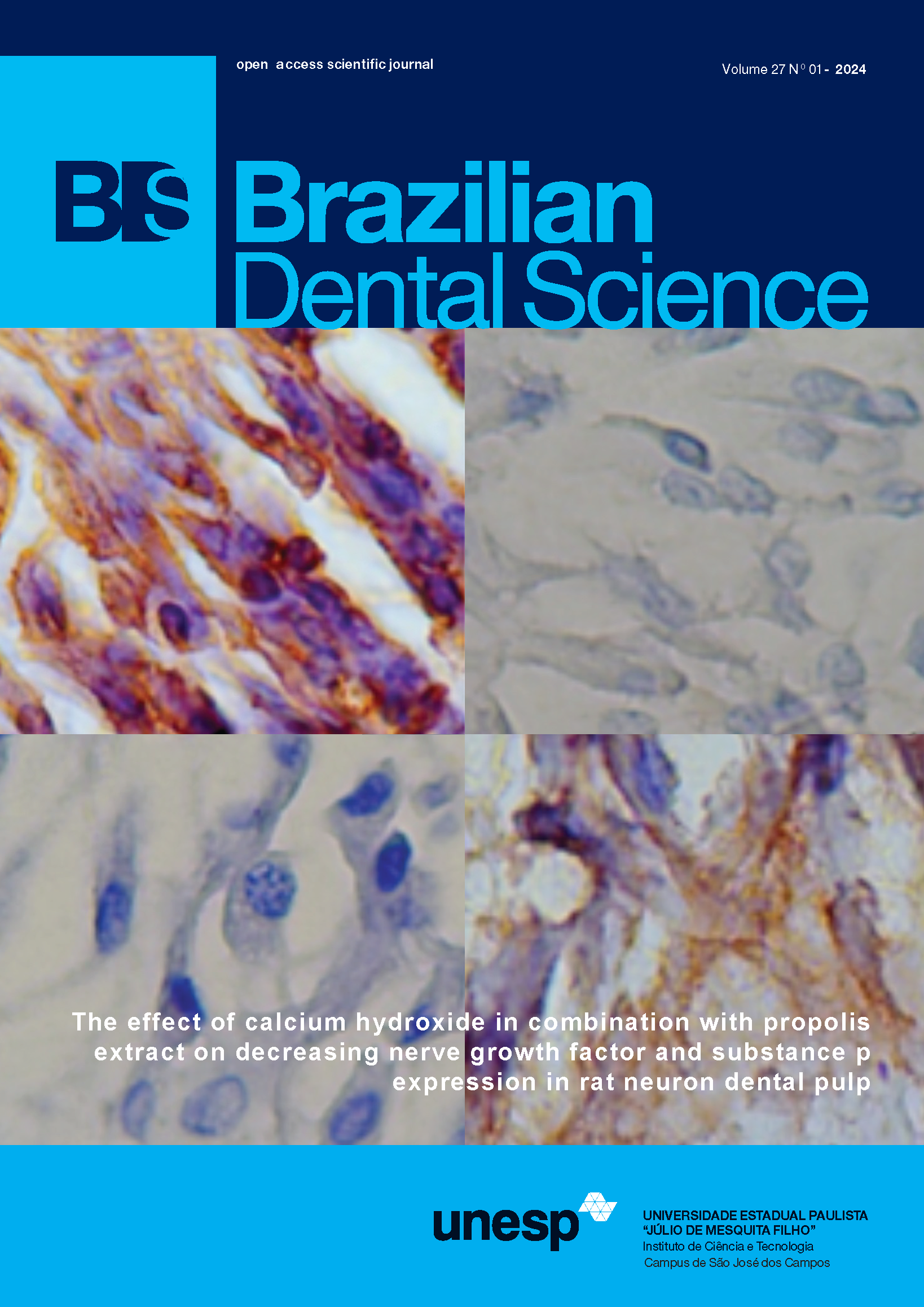
Maxillary osteomyelitis associated with COVID-19: mucormycosis or not? A series of cases
DOI:
https://doi.org/10.4322/bds.2024.e3811Resumo
Aim: A series of cases have been presented involving the oral cavity focusing on the presentation, diagnosis and treatment of mucormycosis that can form a basis for successful therapy. Background: The management of severe coronavirus disease (COVID-19) in conjunction with comorbidities such as diabetes mellitus, hematological malignancies, organ transplants, and immunosuppression have led to a rise of mucormycosis which is an opportunistic infection. Cases Description: The various forms that have been enlisted till date are rhinocerebral, rhino-orbital, gastrointestinal, cutaneous, and disseminated mucormycosis. From the dentistry and maxillofacial surgery perspective, the cases depicting extension of mucormycosis into the oral cavity have been less frequently recorded and thus, require a detailed study. The patients that reported to our private practice had non-tender swelling, draining sinuses and mobility of teeth. A similarity was observed in the clinical signs both in osteomyelitis and mucormycosis. Thus, a histopathological examination was used to establish the definitive diagnosis. Conclusion: Mucormycosis is a life threatening pathology that requires intervention by other branches to make an early diagnosis and commence the treatment. The characteristic ulceration or necrosis is often absent in the initial stage and thus, histopathological examination and radiographic assessment are required to formulate a definitive diagnosis. Early intervention is a necessity to avoid morbidity. The treatment involves surgical debridement of the necrotic infected tissue followed by systemic antifungal therapy. Mucormycosis has recently seen a spike in its prevalence, post the second-wave of coronavirus pandemic in India. It was seen commonly in patients with compromised immunity, diabetes mellitus, hematological malignancies, or on corticosteroid therapy. Mucormycosis invading the palate mostly via maxillary sinus has been less frequently described. In the post-COVID era the features associated with mucormycosis involving oral cavity, should warrant a possible differential diagnosis and managed appropriately.
KEYWORDS
Eschar; Immunomodulation; Mucormycosis; Palatal ulceration; Rhino-Cerebral.
Downloads
Downloads
Publicado
Como Citar
Edição
Seção
Licença
TRANSFERÊNCIA DE DIREITOS AUTORAIS E DECLARAÇÃO DE RESPONSABILIDADE
Toda a propriedade de direitos autorais do artigo "____________________________________________________________________" é transferido do autor(es) para a CIÊNCIA ODONTOLÓGICA BRASILEIRA, no caso do trabalho ser publicado. O artigo não foi publicado em outro lugar e não foi submetido simultaneamente para publicação em outra revista.
Vimos por meio deste, atestar que trabalho é original e não apresenta dados manipulados, fraude ou plágio. Fizemos contribuição científica significativa para o estudo e estamos cientes dos dados apresentados e de acordo com a versão final do artigo. Assumimos total responsabilidade pelos aspectos éticos do estudo.
Este texto deve ser impresso e assinado por todos os autores. A versão digitalizada deverá ser apresentada como arquivo suplementar durante o processo de submissão.